

Based on the best scientific evidence, the following recommendations will help you to maintain a lower risk for developing heart disease and stroke. Please note that the first nine items on the list will work whether you have high cholesterol or not. Item number "10" is for those with high cholesterol or a strong family history of heart disease.
1. Take a multivitamin daily that includes at least 400 mcg (0.4 mg) of Folic acid (also called folate). Some of my favorite multivitamins are: Twin Labs Daily One Caps, NOW Special Two Tablets (not capsules) and GNC Ultra Mega Gold.
2. Take extra Vitamin E daily, at least 400 IU (International Units) and no more than 1000 IU.
3. Take extra Vitamin C daily, at least 500 mg a day, but preferably 500 mg twice a day. Some studies suggest that a form of Vitamin C, called Ester C is superior, but no one knows for sure. If you don’t mind spending a little extra, I recommend it.
4. Another useful vitamin for reducing cholesterol and triglycerides is one of the B Vitamins, called niacin. You can get niacin over the counter. The big problem with niacin is that it can cause a hot, flushing feeling (usually in the neck and face) after taking it. This can be avoided by taking one aspirin tablet (325 mg) about one half hour before taking your niacin. If you don't get flushing, you don't need to take the aspirin. Start with a dose of 250mg of niacin twice a day, and work your way up slowly (250 mg per week) to a total of 750 mg twice a day. When you get up to 1500 mg of niacin daily, it's important that we check a blood test for liver function, as niacin at high doses can cause liver inflammation. I also recommend that you do not take a "long-acting" or "sustained release" or "flush-free" form of niacin, as they have been shown to cause increased risk of liver damage. The best type of niacin to buy is the "fast release" or "quick release" form. This is the safest. Of all brands, a very safe and reliable brand name of fast release niacin is Squibb. If you cannot tolerate the over the counter form, there is a prescription form I can call into your pharmacy for you called Niaspan. The only problem is that this brand is often not covered by your insurance, but it is safe and it does minimize the side effects. Recommended dosing schedule:
Niacin |
AM (with food) | PM (with food) |
| WEEK 1 | 250 mg` | 250 mg |
| WEEK 2 | 500 mg | 250 mg |
| WEEK 3 | 500 mg | 500 mg |
| WEEK 4 | 750 mg | 500mg |
| WEEK 5 | 750 mg | 750 mg |
You should take the niacin with a low-fat snack (apple, whole wheat toast, low-fat yogurt, etc.) or one hour after dinner. Avoiding alcohol, hot drinks and spicy food before taking niacin will minimize the flushing. Flushing usually lasts about 20 minutes and is not a serious side effect. It will not harm you, it is more of a "nuisance" side effect, and will occur less and less frequently over time. After about four months, most patients only experience a flush every two months or so. After one year of niacin, it is a rare occurence.
5. Take 1 baby aspirin tablet a day, that’s 81 mg. You can get the St. Joseph’s chewable or the adult form of baby aspirin. Do not take the aspirin if you are allergic to it, have ulcers, gout, or if you are on any blood thinners like Coumadin, or any anti-inflammatories like Motrin (Ibuprofen) or Aleve (Naprosyn). (Note: If you are already taking one aspirin tablet (325 mg) to prevent flushing from the niacin, you do not need to take an additional baby aspirin.
6. Take 25 grams of fiber a day. The normal diet includes about 10 to 15 grams a day, so you will probably need to supplement with 10 to 15 extra grams of fiber a day. Check your grocery store or health food store for sources. You can try Metamucil, FiberMed Cookies or All Bran cereal sprinkled on foods, but my favorite (and probably the best for you, but the worst tasting, like sawdust) is unprocessed millers bran. Start with 1 to 2 teaspoons a day sprinkled on foods or mixed with water or juice and gradually increase to 1 to 2 tablespoons a day.
You must go slowly because if you increase too quickly, it will cause stomach upset, gas and cramping.
| Unprocessed Miller's Bran | AM | PM |
| WEEK 1 | 1 teaspoon in 8 ounces of water or juice | 1 teaspoon |
| WEEK 2 | 2 teaspoons | 1 teaspoon |
| WEEK 3 | 2 teaspoons | 2 teaspoons |
| WEEK 4 | 3 teaspoons | 2 teaspoons |
| WEEK 5 | 3 teaspoons | 3 teaspoons |
| WEEK 6 | If no stomach upset, 4 teaspoons | 3 teaspoons |
| WEEK 7 | 4 teaspoons | 4 teaspoons |
| WEEK 8 | 5 teaspoons | 4 teaspoons |
| WEEK 9 | 5 teaspoons | 5 teaspoons |
| WEEK 10 | 6 teaspoons | 5 teaspoons |
| WEEK 11 | 6 teaspoons = 2 Tablespoons | 6 teaspoons = 2 Tablespoons |
7. Eat less than 25 grams of saturated fat per day. All
labels on foo ds tell you how much saturated fat there is. Read them and get to
know about
saturated fats. Saturated fats are
ds tell you how much saturated fat there is. Read them and get to
know about
saturated fats. Saturated fats are the ones that come from
animal products like cheeses,
meats, and dairy. Olive oils are fine. For more information regarding a heart healthy
diet, I recommend any of the books by Dean Ornish M.D. He is a well-respected
cardiologist
who did much of the groundbreaking research on how diet and healthy lifestyles can reverse
heart disease.
the ones that come from
animal products like cheeses,
meats, and dairy. Olive oils are fine. For more information regarding a heart healthy
diet, I recommend any of the books by Dean Ornish M.D. He is a well-respected
cardiologist
who did much of the groundbreaking research on how diet and healthy lifestyles can reverse
heart disease.
8. Exercise at least 30 minutes 3 to 4 times a week. If you are out of shape, start with walking. To lose weight, please realize that you need to exercise for at least 60 minutes four to six times a week. That is because the first 30 minutes of aerobic exercise only burns off the sugar stored in your liver and muscles. These sugar stores are called "glycogen stores." Between 30 and 45 minutes, your body transitions from burning glycogen to burning fat. It is only after 45 minutes that you are burning pure fat. This is the when you will benefit most in terms of weight loss. What I tell patients is that you only have to exercise 15 minutes, but you have to walk 45 minutes to get to the gym! The good news is you don’t have to walk 45 minutes back! This 60 minutes does not have to be vigorous. Keep the first 45 minutes at about a heart rate of 100 to 110. At this rate you should be able to carry on a conversation with someone without huffing and puffing. Then pick up the intensity for the last 15 minutes when you are burning off your fat. Good luck. It’s a commitment, but it’s worth it.
9. General advise to reduce risk factors also includes: if you smoke, stop NOW; use alcoholic beverages in moderation (less than 2 drinks per day); if you have high blood pressure, monitor and treat it; if you have diabetes, keep it well controlled.
10. If your cholesterol is high, the cholesterol lowering medicines from the "statin" family have been shown to markedly reduce your risk of future heart disease and stroke. If your total cholesterol is greater than 200 mg %, I may recommend that you begin taking these medicines. Studies show that the lowest risk of heart disease is seen in patients with a total cholesterol around 160 mg %. These medications can help you achieve that level, and they also work to reduce the chance that any existing plaque build-up will break off and rupture (which is what leads to an acute heart attack or stroke). In some cases, if your good cholesterol (HDL) is high enough, it may counteract the bad effects of a high total cholesterol. If I start you on one of these medicines and your lifestyle changes dramatically (i.e. significant weight loss, change in eating habits, etc. ) we can always take you off the medicines and see how your cholesterol does off the medicine. But until those lifestyle changes, I believe it would be safer for you to stay on the medicine. Because these medicines can cause mild, but reversible liver inflammation, we will need to check your liver enzyme level (by a blood test) 12 weeks after starting the medicine. If it is okay, then we will just check it yearly. These medicines are taken once daily at bedtime and they are relatively free of side effects. The most common ones are upset stomach, headache or rash. If you develop strong muscle aches (like when you work out too hard) in all your muscles, you will need to stop the medicine. Also, you should not take erythromycin antibiotics while you are on the cholesterol lowering medicine. If you are on anticoagulants, like Coumadin, your levels need to be monitored carefully.
11. If your cholesterol is high, and you absolutely don't want to be on one of the statin drugs, you can try herbal alternatives. My only caution is that these herbs have not been fully tested to the degree that prescription medications have. They do not undergo the rigorous testing and quality control that pharmaceuticals do. Additionally, though the herbs may lower your cholesterol numbers, they may not have the beneficial plaque stabilizing properties that the statin drugs do. So your cholesterol may come down, but you may not get the same overall protection you would from the statin drugs. Also, herbs can effect your liver and we still need to monitor your liver function tests via a blood test to make sure these herbs are safe for you. I recommend rechecking your cholesterol and your liver function tests after being on the herbs for three months, and at that time, you can call my office for a lab slip or to schedule a blood draw. All that said, if you still prefer an herbal approach, here are some recommendations:
1) Red Yeast Rice: You can purchase this pill at Mother's Market or GNC and the recommended dosage is usually 600mg twice a day. There is an extended release form (Nature's Plus Extended Release) at Mother's that is only once a day, but my preferred brand is by Soloray and that one is 600mg (1 pill) twice a day. If you're terrible at taking pills, you can take both pills together with your evening meal.
Red Yeast Rice is a Chinese herb developed in about 800 A.D. that has properties similar to the statin drugs along with other natural antioxidants and other compounds. Red Yeast Rice appears to have minimal side effects, though muscle aches, rashes and liver function elevations are possible. Some authorities advise limiting excessive amounts of grapefruit juice with Red Yeast Rice, as it may theoretically cause elevation of the statin levels and subsequent increased risk of side effects. Overall, Red Yeast Rice is considered a very safe herb with fairly dramatic cholesterol lowering abilities. It will lower the total cholesterol as well as raise the HDL cholesterol. To be safe, we should check your cholesterol and liver functions after 3 months, so call the office for a lab slip or blood draw.
For more information about Red Yeast Rice, read:
http://www.ajcn.org/cgi/content/full/69/2/231
http://www.cholesterolbusters.com/cholestene-red-yeast-rice.html
2) Cholnixx. For more information on how Cholnixx works, visit: http://www.myherbalrx.com/products/FAQ/chonixxfaq.htm You can visit their website at: myherbalrx.com for ordering information or call 1-800-769-4372 (HERB) if you have more questions about the product. At this time, Cholnixx is only sold on their website location, so no local stores carry this product. These herbs will probably not be covered under your prescription benefit plan. We should also check your cholesterol and liver functions after 3 months on Cholnixx as well, so give us a call.
3) Gugulipid: This herb is an effective lipid-lowering agent, which lowers total cholesterol, lowers LDL (bad) cholesterol, lowers triglycerides and raises HDL (good) cholesterol. It is very safe and has been scientifically studied. There are many brand names, they all contain guggulsterones. In particular they should contain Z-guggulsterone and E-guggulsterone to be effective. Typically cholesterol levels will drop 14-27% in a 4 to 12 week period and triglyceride levels will drop 22-30%. Clinical studies demonstrate that a daily dose of about 75 to 100 mg of guggulsterone a day is effective. This is usually administered as: one pill three times a day. For a 4% guggulsterone content, the most effective dose is about 500 to 600 mg three times a day. Some website references are:
http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=7848901&dopt=Abstract
http://www.doctorphyto.com/Library/Botanicals/GHI_herbs/Gugulipid.htm
http://www.tnp.com/encyclopedia/substance/57/
http://www.cdriindia.org/gugulipid.htm
http://www.sabinsa.com/products/gugul_paper.htm
4) Cholestatin: This herbal can be purchased at Mother's and most health food stores. These plant sterols help to decrease the absorption of cholesterol from the foods that you eat. The exact dosage varies depending on the brand name, so follow the label's recommendations. Again, as with the other herbals, we should check your cholesterol and liver function tests after you have been on the product for 3 months, so we can assess if it is working or if there are any adverse effects on the liver. Some references are:
http://www.vibranthealth.org/cholestatin5.htm
Additionally, I want you to know that I have no financial interest in Cholnixx, Gugulipid, Red Yeast Rice, Cholestatin or any of the products mentioned here. I do not receive any money or any benefits or any multi-level marketing proceeds from any product I ever mention. My interest is only in what works and what is healthy for you.
All of the above vitamins (except Cholnixx) are probably least expensive to obtain at a good health food store, like Mother’s Market (17th Ave. in Costa Mesa, or Jamboree & Michelson). Ralph’s usually carries Twin Labs products. Also GNC and Apple-A-Day carry most of these brands.
SPECIAL NOTE: The following section is for those interested in a deeper understanding of the mechanisms whereby elevated blood lipids contribute to the process of atherosclerosis and increased risk of heart disease and stroke. Though it is somewhat technical, please make an effort to read through the material below, so that you will have a better understanding of why the many treatment recommendations listed above are truly beneficial.
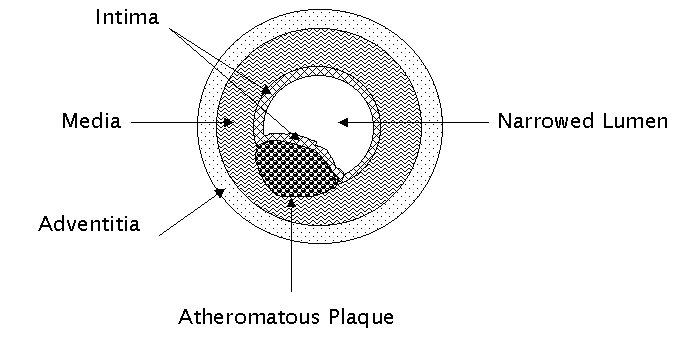
A basic understanding of how fatty elements in the bloodstream build up inside artery walls is important in understanding how certain medications, foods and vitamins work in reducing your risk of heart disease and stroke. When fatty elements accumulate just beneath the intima (innermost layer) of the artery wall, they begin to cause a narrowing of the lumen of the artery. This process is called atherosclerosis, which is a form of arteriosclerosis, commonly known as "hardening of the arteries." (Although more technical than you really need to know, for those of you interested, atherosclerosis is actually one of three main forms of arteriosclerosis, which is a generic term for blood vessel disease in which there is abnormal thickening and loss of elasticity in the artery. )
The fundamental hallmark of atherosclerosis is the atheromatous plaque, (commonly referred to as a plaque). Plaques are really a collection of three elements: 1) blood cells (including white blood cells, platelets and vascular smooth muscle cells (SMC) 2) connective tissue fibers and 3) lipids (mainly cholesterol and triglcerides) that build up beneath the intima (innermost layer) of the artery wall. As these elements build up just beneath the intima, they begin to push the intima in towards the lumen of the artery and cause "blockage" of the blood flow.
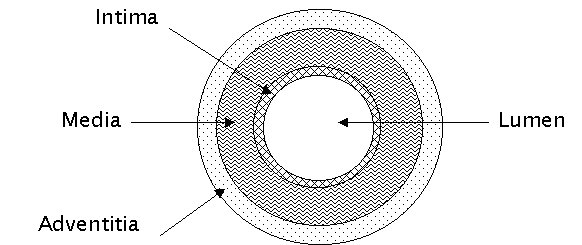
Let's digress to look at the anatomy of a healthy artery. Arteries are like a tube made of up three layers: 1) the intima: a thin innermost layer made up of endothelial cells and a thin elastic membrane 2) the media: a relatively thick middle layer made up of smooth muscle cells and strong elastic fibers and 3) the adventitia: an outer layer made up mostly of connective tissue (which is the "glue" that holds the cells of the body together.)
There is a common misunderstanding that plaque builds up like debris along the inner wall of the artery, like calcium deposits on the inside of a copper pipe. This is not true. Plaque represents a buildup of blood cells, connective tissue fibers and lipids that rest just beneath the intimal layer of the artery, between the media and the intima.
When plaque builds up inside the artery well, the artery becomes unhealthy and serious consequences may develop. There are two main ways in which plaque buildup can cause problems that lead to stroke and/or heart attack.
1) If the artery is relatively small, the buildup of a large plaque can increasingly narrow the lumen of the artery, resulting in decreased blood flow and possibly, eventually, complete occlusion of the vessel lumen. This would essentially cut off all blood flow and oxygen to the tissues "downstream" from the blockage, leading to cellular damage and destruction.
2) The plaque may become "unstable" and rupture into the lumen of the artery, releasing cellular and fatty elements into the lumen of the artery, where they initiate an internal clotting process and abruptly block off the flow of blood. This process happens quickly and can be catastrophic.
There are several ways in which a plaque may become unstable and rupture into the lumen of the artery. They are:
In advanced disease, plaques may become calcified, causing the plaque itself and the intimal layer overlying it to become brittle and fragile, which leads to cracking or rupture of the intima.
The force of the blood flow through the arteries or certain harmful chemicals in the bloodstream may lead to ulceration or irritation of the intimal lining, which causes fissuring of the intima down into the plaque, thereby releasing the harmful contents of the plaque into the lumen.
Small capillary blood vessels within the plaque itself may "leak" causing the plaque to expand rapidly, like an overfilled water balloon, exploding through the intima into the lumen of the artery.
Damage to the intimal lining adjacent to a bulging plaque may cause a lack of integrity in the endothelial cells that make up the intima, allowing blood from the lumen of the artery to flow in through the intima and down into the plaque itself, leading to the same exploding water balloon situation as described above.
Some patients have difficulty understanding the idea of a ruptured plaque, but just think of what happens when you get an external cut, like a small cut on your hand. When you cut yourself, that cut initiates a clotting process, whereby clotting factors and platelets begin to coagulate, forming a clot that stops the flow of blood. This is a miraculaous and wonderful mechanism to keep us from bleeding to death every time we get a little nick or scrape. However, when this process occurs from an "internal cut" inside the artery wall, the process is devastating, abruptly stopping the flow of blood to vital heart and/or brain tissue.
What Causes Plaque To Build Up In The Arteries In The First Place?"
The most accepted theory is called the "Response-to-Injury" hypothesis. This hypothesis states that chronic or repeated injury to the endothelial cells of the intima, lead to increased permeability. This increased permeability creates tiny "holes" in the intimal layer, which allow blood cells and lipids (cholesterol and triglycerides) from the blood stream to migrate through the intima, where certain chemical factors cause the formation of the atheromatous plaque.
The main factors that seem to cause the repeated injury to the endothelial cells include:
High cholesterol and/or high triglycerides are the most universally acknowledged cause of increased plaque buildup. In particular, when low density lipoprotein (LDL), the so called "bad cholesterol" becomes oxidized in the blood stream, it is damaging to the endothelial lining of the intima and may begin the process of atheromatous plaque development.
Cigarette smoke which leads to circulating bloodstream toxins, low oxygen levels, carbon monoxide and other chemicals that damage the endothelial lining.
Certain viruses can cause damage to the endothelium.
High levels of certain chemicals in the blood, particularly homocysteine, can be toxic to the endothelial lining.
High blood pressure may cause increased turbulence of blood flow which causes a shearing stress on the endothelial lining, leading to damage and subsequent increased permeability.
Diabetes, through unknown processes, leads to endothelial damage.
Increasing age can lead to "wear and tear" of the endothelial lining.
Certain hereditary genetic factors may cause endothelial damage.
Certain drugs, such as birth control pills, caffeine and others may lead to endothelial damage.
Increased levels of uric acid from gout, or thyroid disorders may lead to endothelial damage.
How Can I Put This Knowledge Of What Causes Atherosclerosis To Practical Use?
The use of antioxidants is critical in decreasing the risk of heart disease and stroke. Though antioxidants do not decrease the actual cholesterol levels, they do prevent the oxidation of the LDL cholesterol particle, which is extremely toxic to the endothelial lining and is a major player in the development of the atherosclerotic plaque. Therefore, by increasing your levels of antioxidants in the blood, you can help prevent the oxidation of LDL and minimize the risk of plaque formation. Antioxidants may also stabilize the plaques that are already there, preventing them from rupturing.
The use of a daily baby aspirin helps to "thin" the blood and minimize the chance that if a plaque does rupture into the lumen, that it will develop into a large clot, thereby blocking the blood flow in the arterial lumen. Needless to say, this is something we definitely want to prevent, if God forbid, a plaque should rupture or ulcerate.
The use of the statin drugs like Lipitor, Baycol, Pravachol, Zocor, etc. is critical for two important reasons. The first is that they lower the level of LDL cholesterol and triglycerides dramatically, thereby decreasing the risk that endothelial damage will occur and decreasing the risk that new plaque will form. The second beneficial effect of these drugs is that they help stabilize existing plaque, helping to prevent it from rupturing. This is sometimes called "endothelial stabilization," meaning that, by some miraculous event, these drugs help prevent the damaging plaques that have already built up from causing further damage. This endothelial stabilizing effect was a totally unexpected finding but one that makes these drugs one of the truly life saving, miraculous discoveries of modern medicine. This is the reason that even patients who have normal cholesterol levels, but a strong family history of heart disease or stroke, can reduce their risk of a future heart attack or stroke by up to 30%.
When you have more than one risk factor for heart disease, such as high blood pressure and a strong family history of heart disease, your risk for developing heart disease or stroke increases greatly. For this reason, in patients who have more than one risk factor, I will often recommend a more aggressive approach and start a statin medication like Lipitor much sooner. Risk factors include: diabetes, hypertension, being overweight, strong family history and the like. In these cases, my goal is to get your LDL cholesterol level below 110 mg %, even though anything less than 130 mg% is considered normal. In other words, with multiple risk factors, we must raise the standards in order to prevent the risk of heart disease and stroke and protect your health.
For example, in the Framingham heart study, patients with three risk factors (high cholesterol, high blood pressure and smoking) had a heart attack rate seven times greater than when no risk factors were present. Two risk factors increased the risk fourfold.
What Are My Treatment Goals For Reducing My Cholesterol Levels?
The answer is, it depends! If you have no other risk factors for heart disease except high cholesterol or high triglycerides, then the goal is to have the total cholesterol less than 200 mg% and the LDL cholesterol (the "bad cholesterol") less than 130 mg%, with the triglycerides less than 150mg%.
If you have other risk factors, such as a strong family history of heart disease (like a father, mother, brother, grandparent, uncle or aunt, with a heart attack, stroke or bypass surgery in their 50's or 60's), diabetes, obesity (more than 15 to 20 pounds overweight), evidence of atherosclerosis on x-rays or ultrafast CT scan of the heart; then your total cholesterol should be less than 180 mg%, with the LDL cholesterol less than 100 to 110 mg%, and triglecerides less than 150 mg%. Note that in some cases if your HDL (the "good cholesterol" is very high i.e. greater than 50 to 60 mg% ) and your cholesterol/HDL risk ratio is less than 3.5 to 4.5, you may be able to get by with an LDL cholesterol of 110 - 130 mg%.
How Do I Interpret My Cholesterol Results?
There are two main parameters we measure in the blood, which help us determine your risk for heart disease. They are:
1) LDL cholesterol: This is also known as the "bad cholesterol" or low density lipoprotein
2) The Cholesterol/HDL Ratio (Also called the "Risk Ratio"): This number is calculated by taking the total cholesterol and dividing by the HDL cholesterol. For example: if your total cholesterol is 200 mg% and your HDL cholesterol is 40 mg%, then your cholesterol/HDL ratio (also known as "risk ratio") is 5.0
If your LDL cholesterol is less than 130 mg% and your cholesterol/HDL ratio is less than 5.0 (if you're a man) and less than 4.4 (if you're a woman), then we consider your values to be normal, and you should have nothing to worry about, unless you have a strong family history of heart disease, or some other complicating risk factors.
If either your LDL cholesterol is greater than 130 mg% or your cholesterol/HDL ratio is greater than 5.0 (for a man) or 4.4 (for a woman), then further investigation needs to be done to decide if treatment is necessary. When you fall into this category, we have what is known as "conflicting data" and no one really knows what to do without more information. Imagine if you were staking out a house for suspicious activity, and you had two teams of officers on duty, one looking at a house from the front and the other team viewing the house from the back. If your LDL is high, but your risk ratio is normal, it is as if the house looks all quiet from the front, but there seems to be some activity going on in the back of the house. In this case, it is necessary to send a team to further investigate the situation. This is what is necessary when either your LDL or your cholesterol/HDL risk ratio is abnormal.
How Do I Further Investigate The Problem?
There are a few things that can help, but first let me reframe the question. What we really want to know in this situation is, "Can you just follow the recommended dietary and exercise changes, or do you really need to be on medication?" No one wants to take medication unless it is absolutely necessary. Factors that would lead me to put you on medication include:
A strong family history of heart disease, i.e. relatives who had a stroke or heart attack in their 50's or 60's
Diabetes
High blood pressure
You are a smoker and are not going to quit
You are in your 50's or 60's
You are inactive or unable to exercise regularly
You eat fatty foods
You drink a lot of caffeine and are unable or unwilling to quit
There are now some other objective tests that can be done to determine whether you need to be on medication or not. The most recent test is called the Ultrafast CT Scan for Coronary Calcium. This test allows an image of the coronary arteries of the heart, where plaque may build up. One drawback of the test is that it only detects calcium in the atherosclerotic plaques. Many plaques may never calcify, so if the test is totally normal, we still aren't completely sure that there is no plaque buildup. However, if the test does show significant calcifications in the coronary arteries, then we can safely assume that the atherosclerotic process is in progress and we should treat you more aggressively, meaning we will likely start you on the statin medications.
This CT scan is not usually covered by insurance companies and runs about $300 to $450 depending on where you go. You can go to Hoag Hospital (800) 309-9729, or there is a group in Irvine called HeartSavers (949) 786-6600 that does an excellent job. Also, a company called HealthView in Newport Beach (888) 724-VIEW offers this test.
If you have conflicting cholesterol results, this test will help us decide whether you need medication or not. If you have no great objection to being on the statin medications, you can also just decide to "play it safe" and start the medication. In reality, these medications are amazingly safe and do indeed save lives. Virtually all of there side effects are reversible, so that if you do develop liver inflammation or a problem from these medications, they will go away when you stop the medication.
Please do not use these medications, however, as a substitute for the healthy dietary and exercise changes that are recommended. They are not a license to eat irresponsibly and ignore necessary and healthy lifestyle changes. These lifestyle changes also afford you great protection from diseases other than cancer, including cancer and immune disturbances. Additionally, the body was meant to move, and good exercise and eating will make you feel healthy, stronger and more vital.
One last point, if you decide to start the medication and within a year or so, you establish a healthy exercise and nutritional routine, lose some weight and just plain get your act together, we can always discontinue the statin medication and recheck your cholesterol off of it, to see if you still require it. That's it for now. I know it's been a rather lengthy discourse, but I hope the above information has helped you.
God bless you and good luck in your efforts for achieving a healthier body.
Return To The Mind/Body Connection Home Page